Welcome to the
Facial, Eye & Body Prosthetics Clinic
At the Johns Hopkins Facial, Eye & Body Prosthetics Clinic, our Certified Clinical Anaplastologists provide patients with non-weight bearing custom-designed rehabilitative prostheses. These devices are used in the treatment of disfigurements caused by trauma, cancer, or developmental differences. Oseeointegration and other new technologies are used for complex cases.
A variety of prosthetic services
Our scope of practice includes prosthetics for the face, eye and body.
Highly Trained Faculty
Our clinical anaplastologists are certified in many areas and are leaders in their specialities
Innovative processes
Access cutting-edge technology, a world-reknowned institution and resources that are unmatched
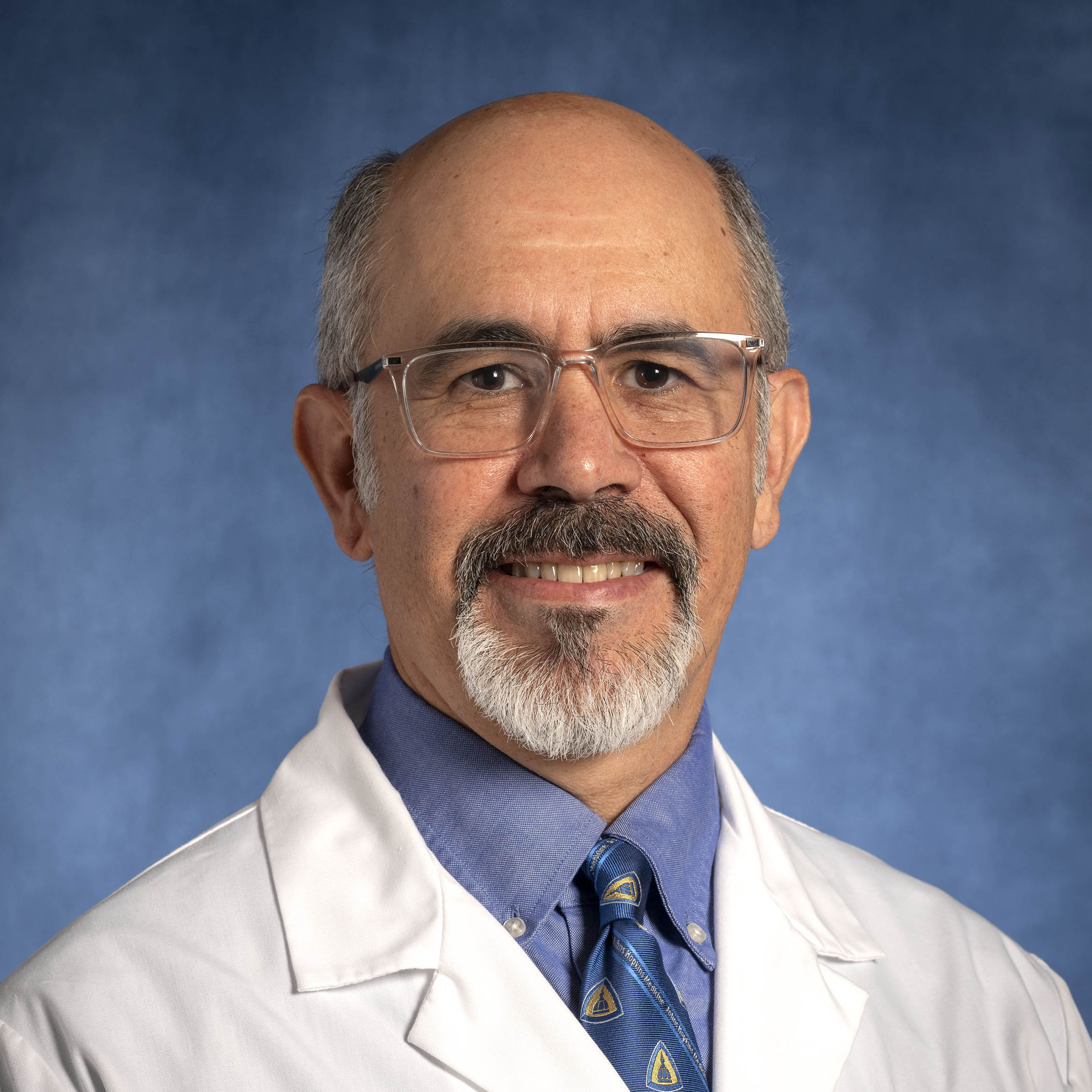
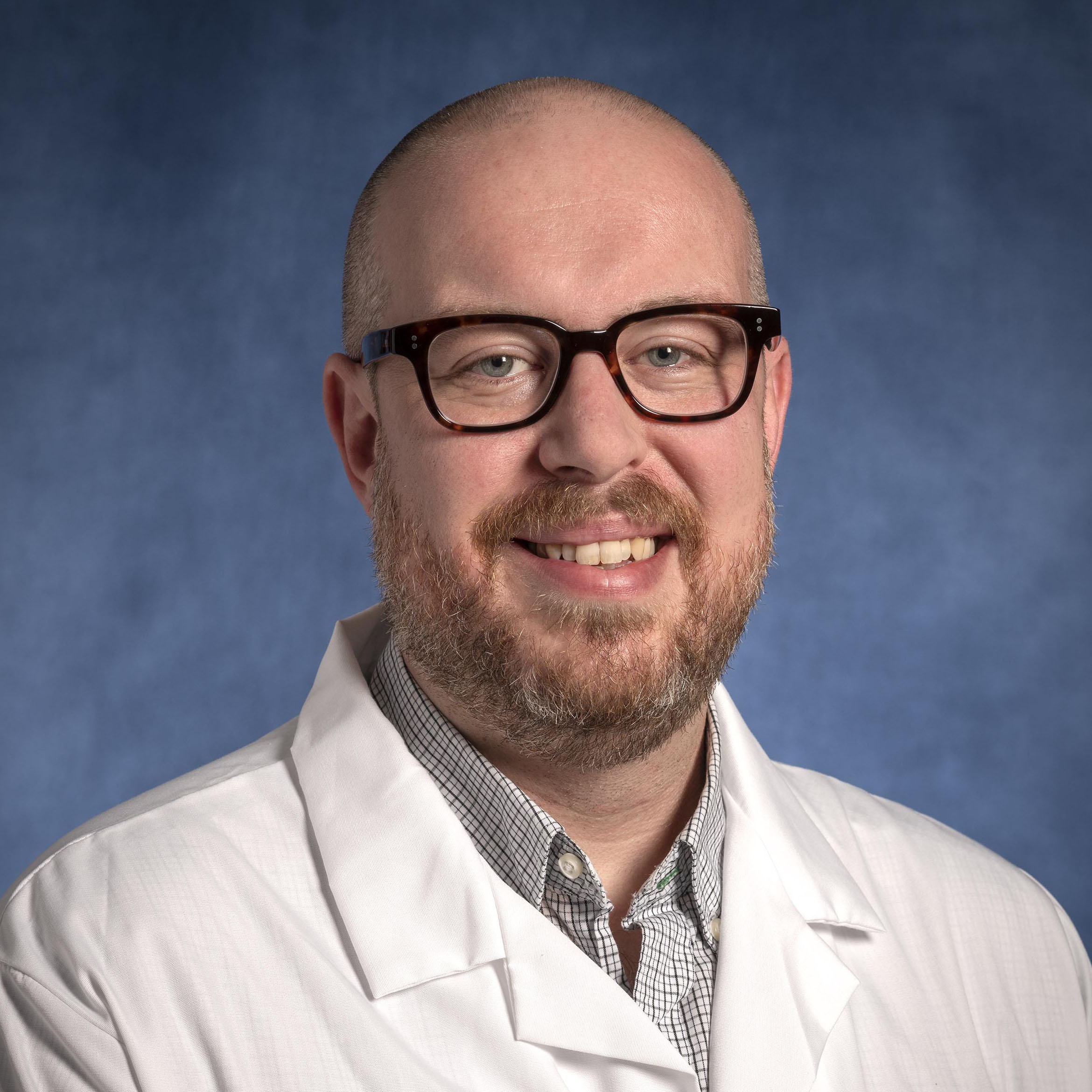
Meet the Team

Carolyn McCloud-Hamm
Senior Medical Office Coordinator
Schedule a Free Consultation
Patients and physicians may arrange for a free consult or referral by calling 410-955-8215.
About Our Providers and Services

The Clinical Anaplastologist
At the Johns Hopkins Facial, Eye & Body Prosthetics Clinic, our Certified Clinical Anaplastologists provide patients with non-weight bearing custom-designed rehabilitative prostheses. These devices are used in the treatment of disfigurements caused by trauma, cancer, or developmental differences.
Patients and physicians may arrange for a free consult or referral by calling 410-955-8215.
The professional that creates the prosthesis is known as a clinical anaplastologist. This is a non-physician provider with varied educational and training backgrounds.
Learn more about our Masters Program in Clinical Anaplastology
The Johns Hopkins Department of Art as Applied to Medicine offers a unique Master of Science Degree Program in Clinical Anaplastology for individuals interested in pursuing education in this field. Program requirements as well as information for applying can be found by clicking the link above. Individuals interested in learning more about the field are also encouraged to review the Education and Training information posted on the International Anaplastology Association (IAA) and the Candidate Handbook information posted on the Board for Certification in Clinical Anaplastology (BCCA).

Prosthetic Rehabilitation
The prostheses a clinical anaplastologist makes are non weight-bearing and are worn externally, on the skin surface to cover, protect, and modify disfigured or missing anatomy in the face, eye or body. These devices are not meant to be “perfect” or “totally indistinguishable.” Instead, they are “realistic enough” to allow the wearer to maintain social interaction while minimizing discomfort. The primary concern is to protect and maximally restore function through a safe and comfortable prosthesis.
Read More
Prostheses address several functional needs such as protecting underlying fragile tissues, closing off an open cavity, warming incoming air, and providing support for eyeglasses. Secondarily, the device should match the remaining anatomy as much as possible, knowing that there are limitations to reproducing living tissue through the use of artificial materials and a process that relies equally on clinical, artistic and technical skills. Other factors, such as secure retention and the ability of the patient to accept and care for the device over the long term, will also contribute to a successful outcome.
A prosthetic treatment plan is generally decided upon through a collaborative effort between the physician, clinical anaplastologist, and the patient. Once the patient has been medically cleared to proceed with treatment, a prosthesis can generally be made over several office visits.
The process involves the following steps: creating a casting of the affected area, sculpting a custom prosthesis out of wax, creating a mold of the sculpted form, casting the final prosthesis in silicone, and externally painting to more closely match a patient’s skin tones. Prostheses can be secured through the use of adhesives, tape, magnets or implantable screws to which a bar and clip or magnet system is attached. The chosen method of retention will affect the length and number of appointments as well as the time frame for delivery of the prosthesis.
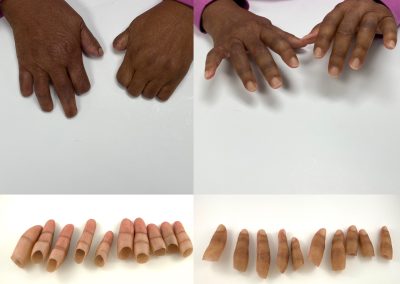
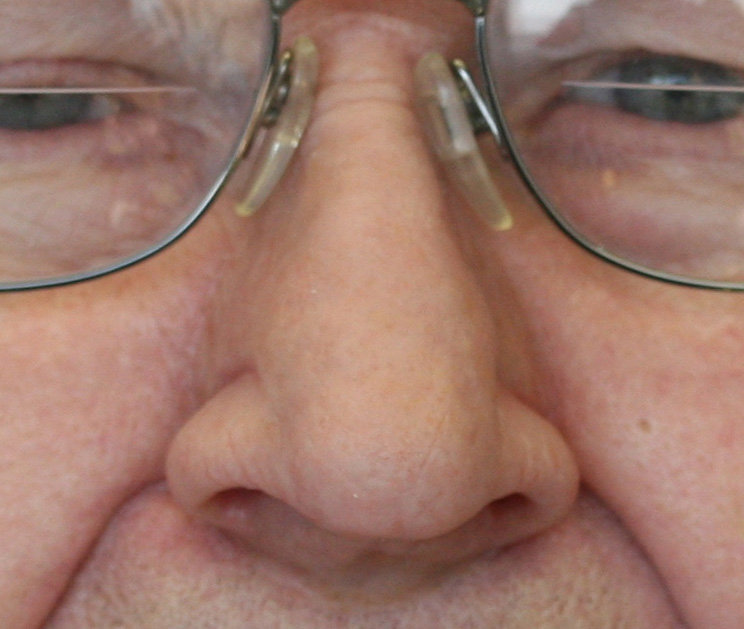
Sample Cases
The kinds of prostheses made by our clinic are broadly categorized into:
- Facial (including orbital, nasal, auricular, and other combinations in the face);
- Ocular (or eye prosthesis),
- Somatic (e.g. Tracheostoma speech appliances, fingers, hands, feet, toes),
- Custom Medical Devices (including custom surgical guides and custom body implants).
All images © JHU, Juan García, or Andrew Etheridge
Frequently Asked Questions
Can I just purchase an already made prosthesis?
Prostheses are custom made for the individual. They are not “off the shelf” items. Several appointments will be needed to create a safe and effective prosthesis that is also realistic in appearance.
Will my medical insurance cover the cost of a prosthesis?
Prostheses are considered durable medical equipment (DME) and are covered by most medical plans, including Medicare, under the DME rider portion of their policy. A Certificate of Medical Necessity is requested from the referring physician to establish the medical need.
When can I start the process of having my prosthesis made?
The patient will need to wait a period of time after surgery for healing to occur before treatment begins. It is preferable that all swelling subsides so the impression that is taken as the first step is accurate. Otherwise the final prosthesis will show noticeable gapping in previously swollen areas. The physician is consulted to determine when the patient is ready for prosthetic treatment.
How long does a prosthesis last before it needs to be replaced?
The expected lifetime of the device is usually 1-3 years for an adhesive retained prosthesis; whereas osseointegrated prostheses tend to last 3-5 years. Since these are separate from the body and made from artificial materials, prostheses can be lost, damaged, or discolored by smoke and UV light. Subsequent remakes can be made using molds which are kept on file for the patient.
How is a prosthesis worn? What is retention?
Prostheses are removed daily, at the end of the day. They are not permanently attached to the site.
Retention (keeping the prosthesis on the body) is a topic of particular concern to the patient. Prostheses should be well retained to the tissues they cover. Various methods of retention with different strengths are available. These include: adhesive, attaching to eyeglasses, using tape and magnets, using anatomical undercuts, and osseointegrated implants.
The retention method is considered during the treatment planning process and is chosen in consultation with the physician and patient based on factors such as age, visual acuity, manual dexterity, sensitivity of skin, and past radiation treatment.
Osseointegrated (OI) retention is considered state of the art. It is easier on the patient because it does not require putting on and removing adhesive daily. The patient simply attaches their prosthesis using a magnet or clip system.
How do I care for my prosthesis?
Prosthetic restoration requires daily care and maintenance procedures. Prostheses are removed on a daily basis, and the skin, osseointegrated implant abutments and prosthesis are cleaned. If required, adhesive is applied and removed on a regular basis.
Request More Information
Juan R. García, MA, and Andrew Etheridge, MFA, both Certified Clinical Anaplastologists, are available to consult with referring physicians and new patients. Fill out the form below or call 410-955-8215 to get started.